Verify patient eligibility
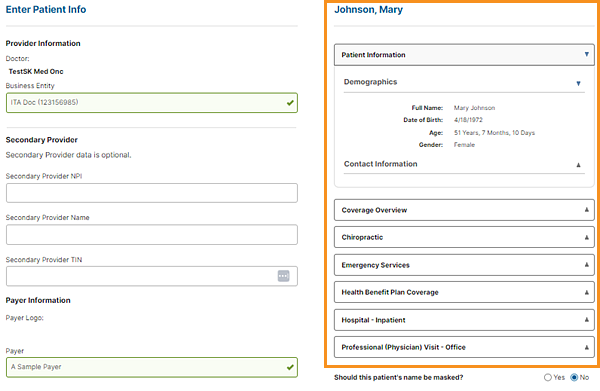
When the user enters a patient into Eviti Connect, we can verify the patient's eligibility to ensure that the user chooses the correct payer and that the patient is covered.
Without verifying eligibility, the user may submit the treatment plan to the wrong payer. Users at that payer's office can view the patient's treatment plan, which violates HIPAA.
Example
If we verify eligibility, the system displays the patient's coverage information in the right panel, after the user enters the patient information and clicks Search.
If the patient isn't covered, the user can't continue entering the treatment plan.
If we don't verify eligibility, the user must enter the patient's address, and your payer confirmation number and group number to continue entering the treatment plan.
Best practice
Verify patient eligibility in Eviti Connect to ensure that the patient is covered, to avoid rework when a user chooses the wrong payer and to comply with HIPAA.
The best practice is to use the real-time X12 270/271 Health Care Eligibility Benefit Inquiry and Response, but you could also send us daily eligibility files.